Motor Abnormalities a Harbinger of Serious Mental Illness? – Medscape

Motor problems in children may be a harbinger of serious mental illness, new research suggests.
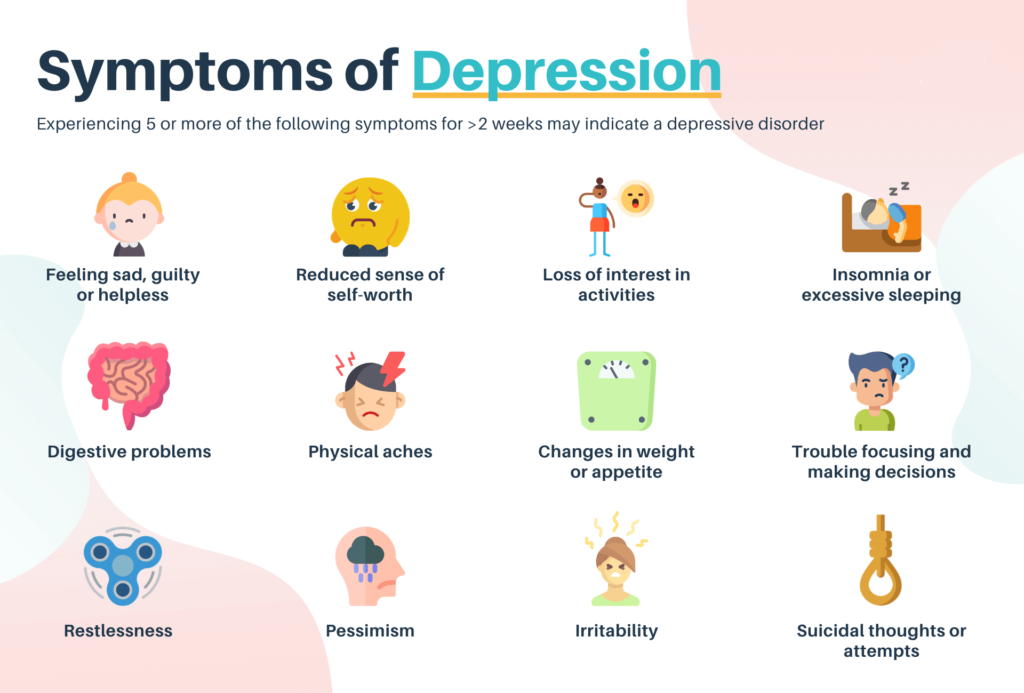
Investigators found that motor abnormalities were twice as common among those who develop psychosis or depression compared to their counterparts in the general population, suggesting that these abnormalities may help predict vulnerability and provide an opportunity for early intervention.
“We have learned there are motor signs that are measurable in adolescence [that are] more prevalent in these disorders,” said lead investigator Katherine S. F. Damme, PhD, Adolescent Development and Preventive Treatment Program (ADAPT), Northwestern University, Chicago, IIllinois,
“This is just scratching the surface of motor signs, but they may have some transdiagnostic vulnerability across these psychopathologies” to which sensorimotor connectivity and motor behaviors “might provide additional insight,” Damme added.
The findings were presented at the virtual Congress of the Schizophrenia International Research Society (SIRS) 2021.
A Core Symptom
There has been a lot of interest in the pathophysiology of psychosis and in detecting it early, said Damme. “It has devastating effects, and early intervention is of great importance,” she added.
However, previous research has typically focused on effect or cognition, rather than on motor signs, despite the fact that motor signs are a “core symptom of both psychosis and depression.”
The prevalence and presentation of motor signs in adolescence, which is a “critical time for identifying these risk markers” because of their proximity to the onset of psychosis, has been understudied, Damme said.
For their study, the investigators gathered motor function data from the Adolescent Brain Cognitive Development Study (ABCD), which included 10,835 children aged 9 to 11 years with broad demographic diversity from 21 sites across the United States.
Overall, 27.6% of the children were reported to have at least one motor sign; approximately 3% were reported to have two or more motor signs.
The most common of these was dyscoordination, which was endorsed by 19.3% of participants. In addition, 8.8% were reported to have had experienced developmental motor delays, 1.5% had psychomotor agitation, and 0.3% had psychomotor retardation.
The investigators determined that 4.6% of participants met the criteria for depression, 2.6% for psychosis, and 1.8% for comorbid psychosis and depression.
Motor signs were much more common among children with depression, psychosis, or both than among those who did not have these conditions; 45.8% reported having at least one motor sign.
Developmental motor delays and dyscoordination occurred at about the same rate in both patients with depression and those with psychosis. Rates were higher among patients with both of these conditions than among those with either condition alone.
In contrast, psychomotor agitation was more common among patients with depression alone and among those with comorbid depression and psychosis than among patients with psychosis alone. The rate of psychomotor retardation was increased among patients with psychosis alone but was less common among patients with comorbidity than in the healthy control group.
Familial Vulnerability
The investigators also assessed participants who had not been diagnosed with a mental illness but who had a family history of depression only (28.9%), a relative with psychosis-like experiences (0.6%), or a family history of both depression and psychosis experiences (1.8%).
Although the effect size was smaller, there was a higher rate of motor signs among participants with a family history of these conditions, Damme said. “Again, we see that it’s elevated across developmental motor delays and at a similar rate in people who have depression and psychosis.”
In addition, psychomotor agitation was linked to depression with psychosis and depression without it.
Sensorimotor connectivity network data for the cohort indicated there was no main effect of diagnosis on corticostriatal connectivity.
However, more depressive symptoms were related to less connectivity (P = .024). There was a similar finding for psychotic-like experiences. The total number of such experiences related to lower connectivity (P < .001).
During the post-presentation discussion, Ian Kelleher, MD, PhD, honorary clinical lecturer in psychiatry at the Royal College of Surgeons, Ireland, Dublin, said he was “surprised” by the finding that the rate of psychomotor retardation was lower among participants with psychosis and depression.
Damme noted that some of the motor sign item ratings came by way of a child interview and that some of these item ratings came from the adults in the children’s lives.
She added that she was not entirely sure whether asking an 8- to 11-year-old in a clinical interview whether they are experiencing motor signs “might be the best way to get at motor slowing.”
Subtle Features
Commenting on the findings for Medscape Medical News, Peter F. Liddle, MD, PhD, professor of psychiatry, Faculty of Medicine and Health Sciences, University of Nottingham, Nottingham, United Kingdom, noted that the “features we’re talking about are pretty subtle.
“What I’ve been wondering about for some time is whether we should be getting video recordings and using machine learning approaches to teach a computer to recognize normal movements vs abnormal movements and particularly facial expression,” said Liddle, who was not involved with the research.
He called the current study “interesting” but noted several factors that affect the potential utility of the findings in predicting outcomes.
First, they “may not be very good for distinguishing schizophrenia from mood disorders; but if the question is simply determining which young person might go on to develop a significant mental disorder, then it may be useful,” Liddle said.
He endorsed the investigators’ conclusion that motor abnormalities may be a transdiagnostic marker. Beyond that, they may be “more useful as a predictor of the likely long-term severity, but that’s my own hypothesis based on my work,” he added.
Another question concerns the sensitivity of motor abnormalities as a predictive marker. With the rate of the abnormalities identified in those who developed psychosis and depression about double the rate in the overall population, “it sounds like those assessors were fairly sensitive…but not all that specific,” said Liddle.
A third issue relates to treatment. “By the time people get sent to a psychiatrist for assessment for possible impending psychotic illness, they’ve often already had medication,” typically an antidepressant or antipsychotic.
“It’s very well established that dopamine-blocking antipsychotics produce hypokinesia and also dyskinesia,” which could then become a confounding factor, Liddle said.
The study was funded by grants from the National Institute of Mental Health. The study authors and Liddle have disclosed no relevant financial relationships.
Congress of the Schizophrenia International Research Society (SIRS) 2021: Abstract 3007091. Presented April 19, 2021.
For more Medscape Psychiatry news, join us on Facebook and Twitter