correcting-altered-brain-circuit-could-tackle-coinciding-obesity-and-depression
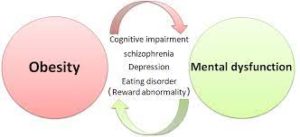
Research has found that obesity and mental disorders such as depression and anxiety seem to often go hand in hand. Researchers at Baylor College of Medicine and collaborating institutions are providing new insights into this association by identifying and characterizing a novel neural circuit that mediates the reciprocal control of feeding and psychological states in mouse models.
Similar to human patients, mice that consumed a high-fat diet not only became obese but also anxious and depressed, a condition mediated by a defective brain circuit. When the researchers genetically or pharmacologically corrected specific disruptions they had observed within this circuit, the mice became less anxious and depressed and later lost excess body weight.
Interestingly, weight loss was not the result of lack of appetite, but of the animals’ change of food preference. Before the treatment, the mice naturally preferred to eat a high-fat diet, but after the treatment, they turned their preference toward a healthier diet with reduced fat and abundant protein and carbohydrates. The findings, published in the journal Molecular Psychiatry, for the first time, not only reveal a key regulatory mechanism for coinciding obesity and mental disorders but also suggest the possibility of pharmacological treatment.
“Reports indicate that 43% of adults with depression are obese and that adults with mental illness are more likely to develop obesity than those who are mentally healthy,” said corresponding author Dr. Qi Wu, a Pew Scholar for Biomedical Sciences, Kavli Scholar and assistant professor in pediatrics-nutrition at Baylor’s Children’s Nutrition Research Center. “Factors such as hormonal dysregulation, genetic deficiency, and inflammation have been proposed to be involved in the connection between obesity and mental disorders. Here we provide evidence that supports the involvement of a neural component.” To investigate the neuronal circuits that could be involved in reciprocally regulating weight gain and depression or anxiety, the researchers provided mice with a high-fat diet. As expected, the animals became obese. They also developed anxiety and depression. In these mice, the team studied the function of neuronal circuits.
“We discovered in normal mice that two groups of brain cells, dBNST and AgRP neurons located in separate brain areas, form a circuit or connection to each other by extending cellular projections,” said co-first author Dr. Guobin Xia, a postdoctoral associate in the Wu lab. “This newly discovered circuit was malfunctioning in mice that were both obese and depressed.”
“Using genetic approaches, we identified specific genes and other mediators that were altered and mediated the circuit’s malfunction in the obese and depressed mice,” said co-first author Dr. Yong Han, a postdoctoral associate in the Wu lab.
“Importantly, genetically restoring the neural defects to normal eliminated the high-fat diet-induced anxiety and depression and also reduced body weight,” Xia said. “We were surprised to see that the animals lost weight, not because they lost their appetite, but because genetically-aided readjustment of the mental states changed their feeding preference from high-fat to low-fat food.”
“Keeping in mind translational applications of our findings to the clinic, we investigated the possibility of restoring the novel circuit pharmacologically,” Wu said. “We discovered that the combination of two clinically-approved drugs, zonisamide and granisetron, profoundly reduced anxiety and depression in mice and promoted weight loss by synergistically acting upon two different molecular targets within our newly identified brain circuit. We consider that our results provide convincing support for further studies and future clinical trials testing the value of a cocktail therapy combining zonisamide and granisetron (or a selection of their derivatives) to treat metabolic-psychiatric diseases.”
Story Source:
Materials provided by Baylor College of Medicine. Originally written by Homa Shalchi. Note: Content may be edited for style and length.